Dementia is one of the most pressing health issues of our time. With people living longer than ever, projections suggest that over 150 million people worldwide could be living with dementia by 2050. Alzheimer’s disease is the most common cause, leading to memory loss, cognitive decline, and personality changes.
For decades, research has centered on two hallmark proteins in the brain: beta-amyloid (Aβ) and tau. While treatments targeting amyloid plaques — such as aducanumab and lecanemab — have gained approval, they come with mixed results and potential risks. Now, attention is shifting toward new approaches, including one that involves an experimental peptide known as PHDP5.
Why Tau Matters in Alzheimer’s Disease

Tau is a protein that normally helps stabilize microtubules — the structures that support communication between neurons. In Alzheimer’s, tau detaches, destabilizes these structures, and eventually forms neurofibrillary tangles. This process blocks the recycling of neurotransmitters and disrupts communication between brain cells.
The buildup of tau tangles is strongly linked to memory loss and learning difficulties in Alzheimer’s. Because of this, scientists believe that targeting tau directly could be key to slowing or even reversing symptoms.
The Promise of Peptide PHDP5
In a new study published in Brain Research, researchers tested PHDP5 in genetically modified mice designed to mimic Alzheimer’s disease. When delivered intranasally — directly through the nose — the peptide reached the hippocampus, the part of the brain most involved in memory and learning.
The results were striking:
- Mice treated with PHDP5 performed significantly better on memory tests compared with untreated mice.
- Their performance was almost identical to healthy control mice, suggesting a restoration of lost learning abilities.
- Brain examination confirmed that PHDP5 reduced tau-related damage and helped restore nerve signaling.
Dr. Emer MacSweeney, CEO of Re:Cognition Health, called the findings “encouraging,” noting that targeting the dynamin-microtubule pathway is a novel approach not seen in current Alzheimer’s treatments.
What Makes This Study Different?
Most existing therapies focus on amyloid plaques, but PHDP5 works through a different mechanism:
- It restores dynamin, a substance that helps recycle neurotransmitters.
- By stabilizing communication at synapses, PHDP5 may reverse memory deficits instead of only slowing decline.
- Importantly, the intranasal route allowed the drug to cross the blood-brain barrier, something that has challenged many experimental treatments.
While the study was conducted in mice, it shows proof-of-concept that tau-related damage can potentially be reversed — a hopeful sign for future human trials.
The Caveats and Cautions
Despite the excitement, experts stress caution.
- Animal studies don’t always translate to humans. Mice can mimic aspects of Alzheimer’s, but the disease in people is far more complex.
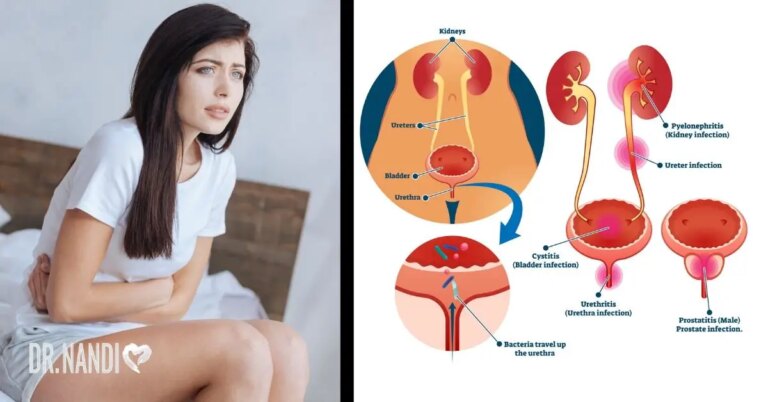
- Safety questions remain. Researchers noted potential risks to the kidneys and nervous system, though intranasal delivery may lower some of these risks.
- Clinical trials are essential. Only through human studies will we know if PHDP5 can truly slow or reverse symptoms in patients.
As Dr. Stefania Forner from the Alzheimer’s Association explained, mouse models “help us understand the biology of disease, but human studies are needed before any real conclusions can be drawn.”
A New Direction in Alzheimer’s Care

If further validated, PHDP5 could represent an entirely new class of treatment. Instead of simply clearing plaques or easing symptoms, it may directly restore communication between neurons.
For patients and families affected by Alzheimer’s, even small gains in memory and cognition can mean a better quality of life. The road ahead is long, but this peptide study offers a glimmer of possibility in an area where progress has often been slow and frustrating.
My Personal RX on Protecting Your Brain Health
Alzheimer’s research is advancing, but prevention and daily care remain your best tools right now. You have the power to support your brain through everyday choices. Here are my recommendations:
- Feed Your Gut-Brain Connection: A healthy gut microbiome supports brain function. Adding a probiotic-based supplement like MindBiotic can help balance gut bacteria, reduce inflammation, and support cognitive health.
- Choose Nutrient-Dense Meals: Plan meals that fuel your brain with antioxidants, healthy fats, and fiber. My Mindful Meals cookbook makes this easier with guided recipes and meal plans.
- Stay Physically Active: Regular exercise improves blood flow to the brain and helps reduce dementia risk. Aim for at least 150 minutes of moderate activity per week.
- Prioritize Sleep: Poor sleep accelerates plaque buildup in the brain. Strive for 7–9 hours of quality rest each night.
- Challenge Your Mind: Keep your brain sharp with puzzles, reading, or learning a new skill. Cognitive engagement is protective.
- Stay Connected: Social interactions boost brain resilience. Maintain strong relationships and participate in community activities.
- Manage Stress: Chronic stress harms both gut and brain health. Practice mindfulness, yoga, or meditation daily.
- Watch Your Numbers: Keep blood pressure, cholesterol, and blood sugar under control. Cardiovascular health is closely tied to brain health.
- Limit Processed Foods: Reduce intake of refined sugars, unhealthy fats, and heavily processed foods that may promote inflammation.
- Stay Informed: Research is evolving rapidly. Keep up with trustworthy medical updates, and always discuss new treatment options with your healthcare provider.









 Subscribe to Ask Dr. Nandi YouTube Channel
Subscribe to Ask Dr. Nandi YouTube Channel









