Nearly 108,000 lives were lost to drug overdoses in the United States in just one year – a statistic that underscores the urgent need for innovative approaches to addiction treatment. But what if the answer to curbing this epidemic lies within us—or more precisely, within our gut?
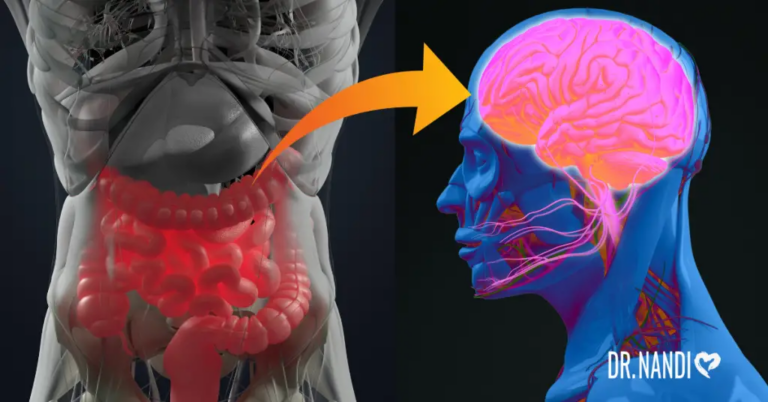
Groundbreaking research reveals that our gut microbiome, the complex ecosystem of bacteria residing in our digestive tract, holds significant sway over our brain’s chemistry and our susceptibility to addiction. This connection suggests that the microorganisms in our gut could be pivotal in controlling cravings and enhancing recovery efforts. As we explore the intricate relationship between gut health and substance use disorders, we discover compelling new possibilities for preventing relapse and supporting long-term recovery.
How the Gut-Brain Axis Is Linked With Substance Use Disorder
Substance use disorders (SUDs) are complex conditions characterized by a chronic reliance on substances like alcohol and opioids, despite harmful consequences to one’s mental, physical, and social health. These disorders are shaped by a combination of socioeconomic, biochemical, genetic, and, notably, microbiological factors. While the brain plays a central role in addiction, the gut microbiome is emerging as a critical player in influencing drug-seeking behaviors.
The gut-brain axis represents a bidirectional communication network where the gut microbiota and the brain interact through metabolic and neural signals. Gut bacteria can produce neurotransmitters such as serotonin and dopamine, which are crucial for mood, cognition, and the brain’s reward mechanisms.
These neurotransmitters are significant in SUDs, as many addictive substances trigger a surge of dopamine in the brain’s reward pathway, leading to the intense pleasure associated with drug use. Over time, as the pleasure diminishes, individuals may repeatedly seek out the substance to recreate these feelings.
Moreover, research suggests that the gut microbiome plays a role in how we perceive rewards, both natural and drug-induced. Substance abuse can alter the gut’s microbial balance, typically reducing beneficial bacteria and increasing pro-inflammatory ones like Proteobacteria. This shift can lead to decreased production of key microbial metabolites like short-chain fatty acids (SCFAs), disrupting the intestinal barrier and causing inflammation. This inflammation can extend beyond the gut, activating immune responses that exacerbate neuroinflammation and potentially affect neuronal activities related to substance tolerance and withdrawal. [1]
Microbial Influence on Opioid Addiction
Opioids, including drugs like morphine, fentanyl, and heroin, are among the most critical public health challenges in the U.S., with around 75% of drug overdose deaths in 2020 involving an opioid. [2]
These substances act by binding to receptors in the central nervous system (CNS) and other areas, such as the gut, reducing pain perception while increasing feelings of pleasure and well-being. This potent combination of effects often leads to addiction and the need for increasingly higher doses, escalating the risk of overdose.
The gut microbiome has been shown to play a significant role in opioid dependence. Research at the University of California, Irvine, highlights how gut microbes influence opioid-seeking behaviors. In studies using a rat model, animals deprived of a diverse gut microbiota through antibiotics demonstrated heightened motivation to self-administer fentanyl. Remarkably, reintroducing short-chain fatty acids (SCFAs), metabolic by-products of bacterial fermentation, mitigated this increased drug-seeking behavior. These findings suggest that the gut microbiome’s composition can directly affect the reward mechanisms triggered by opioid use. [3]
Moreover, opioids impact gut function directly. They are known to cause constipation and other gastrointestinal disruptions by binding to opioid receptors within the gut. These changes correspond with shifts in the gut’s microbial landscape, typically marked by reduced microbial diversity and an increase in potentially harmful bacteria like Staphylococcus and Enterococcus. Such alterations further complicate the challenges of managing opioid addiction.
While the connections between opioid use and the gut microbiome are becoming clearer, the exact mechanisms through which these interactions occur remain under investigation. Unraveling these relationships could be crucial for developing new therapeutic strategies to address opioid addiction effectively.
Understanding Relapse in Addiction Recovery
Addiction recovery is marked by significant challenges, including high rates of relapse, which mirror those of other chronic diseases such as hypertension and diabetes. In 2022, nearly 108,000 individuals in the United States succumbed to drug-involved overdoses, underscoring the persistent threat of substance misuse. Addiction, fundamentally a chronic condition, often includes relapse—defined as a return to substance use after a period of abstinence—as part of the recovery journey.
Relapse rates vary significantly by substance:
- Opioids: Considered exceptionally addictive with relapse rates as high as 91% reported among opioid addicts.
- Stimulants (Cocaine and Amphetamines): Approximately 50% of users relapse within the first year post-treatment, with a 75% relapse rate over five years.
- Alcohol: Among those attempting to quit alcohol use disorder (AUD), only about 25% manage to sustain reduced alcohol intake for more than a year.
- Marijuana: Roughly 49% of individuals treated for marijuana addiction relapse within the first day of its availability post-treatment. [4,5,6,7]
These statistics reflect the complexity of addiction and the critical need for effective treatment and aftercare strategies. Factors such as stress, trauma experiences, depressive symptoms, cravings, and physiological responses like heightened cortisol and adrenaline sensitivity have been identified as significant predictors of relapse. Furthermore, changes in brain structures, such as the medial frontal gray matter and functional responses in the cingulate cortex, also play a role.

Managing Drug Addiction and Preventing Relapse Through the Gut
SUD treatments typically include medications like opioid antagonists, alongside counseling and behavioral therapy. Despite these efforts, statistics have shown that success rates remain low. Emerging research into the gut microbiome suggests a novel approach to enhancing SUD management and reducing relapse risks.
Research has demonstrated the potential of targeting the gut microbiome to mitigate the effects of drug abuse. For instance, studies have shown that probiotics rich in Bifidobacteria and Lactobacillaeae can reverse morphine tolerance in mice. Similarly, a phase 1 clinical trial found that individuals with alcohol use disorder who received fecal microbiota transplants rich in Lachnospiraceae and Ruminococcaceae experienced significant reductions in alcohol cravings. In opioid-dependent models, FMTs have been shown to alleviate withdrawal symptoms, suggesting that microbiome interventions could extend the efficacy of drug therapies and potentially lower the risk of overdose by reducing drug tolerance. [8,9]
Further illustrating the microbiome’s role in addiction, a study published in Neuropsychopharmacology indicated that bacterially derived metabolites can affect drug-seeking behavior. In experiments with rats, those with depleted microbiomes due to antibiotic treatment displayed heightened drug-seeking behavior, especially under conditions of reduced drug availability. This increased activity persisted even after periods of abstinence, indicating a profound influence of the gut microbiome on the propensity for relapse. [10]
These findings highlight the gut microbiome as a promising target for therapeutic interventions in SUDs. By manipulating gut bacteria and their metabolites, it may be possible to modulate the biological pathways involved in addiction and relapse, offering new hope for more effective treatments.
Applying Gut Microbiome Insights to Common Cravings: Alcohol and Sugar
Recent research into the gut microbiome’s impact on substance addiction provides valuable insights that can be applied to more widespread issues, such as alcohol and sugar cravings. By understanding the role of gut bacteria in these cravings, individuals can adopt targeted strategies to potentially alleviate them.
The gut microbiome’s relationship with alcohol cravings suggests that modifying bacterial populations in the gut could help manage these urges. Consuming prebiotic foods that nourish beneficial bacteria, such as those high in fiber, can promote a healthier gut flora balance. For instance, certain bacteria like Lachnospiraceae and Ruminococcaceae have shown potential in reducing the desire for alcohol. Introducing or increasing these bacteria through specific probiotic supplements or dietary changes can be a strategic part of treatment for those struggling with alcohol dependency.
Similarly, the craving for sugary foods can be influenced by the gut microbiome. Diets high in sugar can foster the growth of microbes that increase sugar cravings, creating a self-perpetuating problem. By adjusting your diet to include more complex carbohydrates and fibrous foods, it is possible to shift the gut microbiome away from these sugar-dependent bacteria. Incorporating probiotics that support beneficial bacteria which do not rely on sugar for growth can also help decrease the intensity of sugar cravings.

My Personal RX on Fighting Unhealthy Cravings and Addiction
The gut-brain axis plays a significant role in controlling cravings and potentially addictive behaviors. As a healthcare professional, I emphasize the importance of maintaining a healthy gut to help manage and reduce unhealthy cravings. A well-balanced microbiome can influence mood, decision-making, and even the physiological impulses that drive cravings and addiction. Here are strategic tips to harness the power of your gut health to combat these challenges.
- Incorporate Probiotic and Prebiotic Foods: Foods rich in probiotics and prebiotics help balance the gut microbiome, which is crucial for producing neurotransmitters like serotonin that regulate mood and appetite. Eating a diet rich in fiber (from fruits, vegetables, and whole grains) and fermented foods (like yogurt, kefir, and sauerkraut) can fortify your gut health and potentially reduce cravings.
- Utilize MindBiotic: MindBiotic combines the benefits of probiotics, prebiotics, and Ashwagandha, which not only support digestive health but also enhance stress resilience and mental clarity. By stabilizing the gut-brain axis, MindBiotic can help mitigate the emotional and physiological triggers that lead to cravings and addictive behaviors.
- Stay Hydrated: Often, cravings can be mistaken for dehydration. Before giving in to a sudden craving, drink a glass of water and wait a few minutes. This can help reduce the intensity of cravings and support overall digestive health.
- Follow Heal Your Gut, Save Your Brain: This book provides extensive knowledge on how a healthy gut influences brain function, including the management of cravings and addictive behaviors. Implementing its holistic dietary and lifestyle recommendations can enhance both your gut health and your ability to resist unhealthy impulses.
- Eat Regular, Balanced Meals: Consuming meals at regular intervals throughout the day can stabilize blood sugar levels and prevent the hunger spikes that often trigger cravings. Ensure each meal includes a balance of proteins, fats, and carbohydrates to keep you satiated and nutritionally balanced.
- Manage Stress Effectively: Since stress can exacerbate cravings and addictive behavior, managing stress through mindful practices such as yoga, meditation, or deep breathing can be beneficial. These activities not only reduce stress but also enhance gut health by moderating the body’s stress response.
- Avoid High-Sugar and Processed Foods: These foods can disrupt the balance of your gut microbiome and spike blood sugar levels, leading to increased cravings. Opt for whole foods with low glycemic indices to maintain a more stable gut environment and reduce craving episodes.
- Exercise Regularly: Physical activity can modulate gut health positively and reduce cravings by releasing endorphins, the body’s natural mood elevators and painkillers. Regular exercise also helps in maintaining a healthy weight, which can reduce the risk of craving-induced eating.
- Get Adequate Sleep: Lack of sleep can affect the gut microbiome and increase cravings, especially for unhealthy foods. Aim for 7-9 hours of quality sleep per night to help maintain the integrity of your gut flora and support overall health.
- Consider Cognitive Behavioral Therapy (CBT): For those struggling with significant cravings or addictive behaviors, CBT can be an effective treatment method. It helps modify behavior by addressing the underlying thought patterns and emotions that contribute to cravings.
Sources:
- García‐Cabrerizo, R., Carbia, C., O´Riordan, K. J., Schellekens, H., & Cryan, J. F. (2020). Microbiota‐gut‐brain axis as a regulator of reward processes. Journal of Neurochemistry, 157(5), 1495–1524. https://doi.org/10.1111/jnc.15284
- Understanding the opioid overdose epidemic. (2024, November 1). Overdose Prevention. https://www.cdc.gov/overdose-prevention/about/understanding-the-opioid-overdose-epidemic.html
- Ren, M., & Lotfipour, S. (2022). Antibiotic knockdown of gut bacteria Sex-Dependently enhances intravenous fentanyl Self-Administration in adult sprague Dawley rats. International Journal of Molecular Sciences, 24(1), 409. https://doi.org/10.3390/ijms24010409
- Kadam, M., Sinha, A., Nimkar, S., Matcheswalla, Y., & De Sousa, A. (2017). A Comparative Study of Factors Associated with Relapse in Alcohol Dependence and Opioid Dependence. Indian Journal of Psychological Medicine, 39(5), 627–633. https://doi.org/10.4103/ijpsym.ijpsym_356_17
- Understanding relapse and the risks | Hazelden Betty Ford. (n.d.). https://www.hazeldenbettyford.org/articles/relapse-risks-stats-and-warning-signs
- MacNiven, K. H., Jensen, E. L. S., Borg, N., Padula, C. B., Humphreys, K., & Knutson, B. (2018). Association of neural responses to drug cues with subsequent relapse to stimulant use. JAMA Network Open, 1(8), e186466. https://doi.org/10.1001/jamanetworkopen.2018.6466
- Haney, M., Bedi, G., Cooper, Z. D., Glass, A., Vosburg, S. K., Comer, S. D., & Foltin, R. W. (2012). Predictors of Marijuana relapse in the human Laboratory: Robust impact of tobacco cigarette smoking status. Biological Psychiatry, 73(3), 242–248. https://doi.org/10.1016/j.biopsych.2012.07.028
- Zhang, L., Meng, J., Ban, Y., Jalodia, R., Chupikova, I., Fernandez, I., Brito, N., Sharma, U., Abreu, M. T., Ramakrishnan, S., & Roy, S. (2019). Morphine tolerance is attenuated in germfree mice and reversed by probiotics, implicating the role of gut microbiome. Proceedings of the National Academy of Sciences, 116(27), 13523–13532. https://doi.org/10.1073/pnas.1901182116
- Bajaj, J. S., Gavis, E. A., Fagan, A., Wade, J. B., Thacker, L. R., Fuchs, M., Patel, S., Davis, B., Meador, J., Puri, P., Sikaroodi, M., & Gillevet, P. M. (2020). A randomized clinical trial of fecal microbiota transplant for alcohol use disorder. Hepatology, 73(5), 1688–1700. https://doi.org/10.1002/hep.31496
- Meckel, K. R., Simpson, S. S., Godino, A., Peck, E. G., Sens, J. P., Leonard, M. Z., George, O., Calipari, E. S., Hofford, R. S., & Kiraly, D. D. (2023). Microbial short-chain fatty acids regulate drug seeking and transcriptional control in a model of cocaine seeking. Neuropsychopharmacology, 49(2), 386–395. https://doi.org/10.1038/s41386-023-01661-w










 Subscribe to Ask Dr. Nandi YouTube Channel
Subscribe to Ask Dr. Nandi YouTube Channel









