Your immune system works around the clock to keep you safe. It fights off bacteria, viruses, and other harmful invaders every single day. But what happens when that same defense system turns its weapons inward and attacks your own healthy cells? Millions of people around the world know that answer too well. Conditions like lupus, rheumatoid arthritis, and type 1 diabetes all stem from an immune system gone rogue. For decades, doctors and scientists searched for answers about why the body would sabotage itself. In 2025, three scientists earned the Nobel Prize in Physiology or Medicine for cracking a piece of that puzzle. And their discovery could change how we treat some of the most stubborn diseases on the planet.
Your Immune System Has a Secret Police Force
Most people think of their immune system as a simple army. Invaders come in, soldiers go out, and the battle begins. But your immune system is far more complex than that. It must identify millions of threats while also knowing exactly which cells belong to you and which do not.
Every day, your immune system protects you from thousands of different microbes trying to invade your body. Many of these microbes have even developed ways to look like human cells as camouflage. So the question becomes: how does your immune system tell friend from foe?
Your body relies on a process called immune tolerance to make those decisions. One part of that process happens in an organ called the thymus, which sits in your chest. Inside the thymus, T cells (a type of white blood cell) go through a training program. Cells that might attack your own tissues get eliminated before they can cause harm. Scientists call that process central tolerance, and for a long time, most researchers believed it was the only safety net your body needed. But three scientists proved everyone wrong.
Swimming Against the Current: Sakaguchi’s Bold Bet
Back in the 1990s, a Japanese immunologist named Shimon Sakaguchi made a gutsy move. While most of his peers had given up on an old theory about immune cells that could suppress other immune cells, Sakaguchi kept digging.
Earlier researchers in the 1970s had proposed that a special group of T cells might exist with the power to calm down the immune response. Scientists called them suppressor T cells. But early experiments failed to prove they were real, and the scientific community lost interest. Most people moved on. Sakaguchi did not.
Working at the Aichi Cancer Center Research Institute in Nagoya, Japan, Sakaguchi ran a series of experiments on mice. He focused on helper T cells produced in the thymus, identified by a surface protein called CD4. He noticed something that others had missed: not all CD4 T cells acted the same way. Some carried an additional surface protein called CD25. And those CD25 cells appeared to be the key to keeping the immune system from attacking the body.
When Sakaguchi removed T cells carrying CD25 from mice, the results were dramatic. Multiple organs suffered white blood cell attacks, causing severe inflammation in the thyroid, stomach, pancreas, and other tissues. He published his findings in 1995 in a paper that, at first, did not attract much attention. But Sakaguchi had just identified a brand new class of immune cells. He named them regulatory T cells.
Scurfy Mice and a Gene Called Foxp3
While Sakaguchi was building his case in Japan, two researchers in the United States were about to make a discovery that would connect all the dots.
Mary E. Brunkow and Fred Ramsdell worked at Celltech Chiroscience, a biotech company focused on autoimmune disease therapies. They were studying a strange strain of mice known as scurfy mice. Born with scaly, crusty skin and swollen lymph nodes, these mice lived only a few weeks before dying from overwhelming immune attacks on their own bodies.
Brunkow and Ramsdell wanted to know why. By comparing genes in healthy mice and scurfy mice, they identified a mutant gene responsible for the autoimmune destruction. They named it Foxp3. Even more striking, they found that mutations in the human version of that same gene caused a severe autoimmune condition called IPEX (immune dysregulation, polyendocrinopathy, enteropathy, X-linked syndrome).
In 2001, Brunkow and Ramsdell published their findings, and the field of immunology took notice. For the first time, scientists had a genetic explanation for why some immune systems lose control.
Connecting Two Breakthroughs Into One Big Picture
Two years after Brunkow and Ramsdell published their work on Foxp3, Sakaguchi made the connection that tied everything together. He proved that the Foxp3 gene controls the development of regulatory T cells, the very cells he had discovered back in 1995.
In simple terms, Foxp3 acts as a master switch. When it works, your body produces regulatory T cells that patrol the immune system and keep other immune cells from attacking your own tissues. When Foxp3 breaks, those peacekeepers never develop, and the immune system runs wild.
With that connection made, a once fringe theory became accepted science. Regulatory T cells were real; they had a clear genetic basis, and their absence could explain a wide range of autoimmune diseases.
Why Should You Care About Regulatory T Cells?
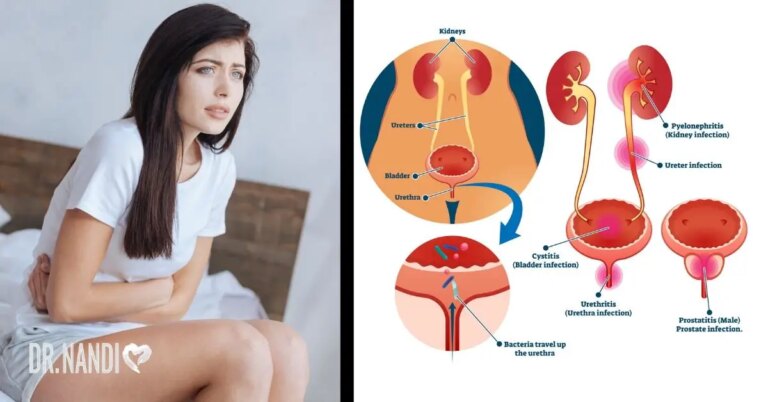
If you or someone you love lives with an autoimmune condition, these findings matter. Autoimmune diseases affect an estimated 50 million Americans alone. Conditions like rheumatoid arthritis, lupus, multiple sclerosis, and type 1 diabetes all share a common thread: the immune system attacks healthy tissue instead of protecting it.
Before these discoveries, treatments for autoimmune diseases focused on suppressing the entire immune system. Drugs like corticosteroids and immunosuppressants can reduce symptoms, but they also weaken your body’s ability to fight infections. It is like turning off your home security system because it keeps setting off false alarms. You stop the noise, but you also lose your protection.
Regulatory T cells offer a smarter approach. Instead of shutting down the whole immune system, scientists are now working on therapies that boost or repair these specific peacekeeper cells. Over 200 clinical trials are testing treatments based on peripheral immune tolerance, according to the Nobel Committee.
From Lab Mice to Real Patients
Several companies and research teams are already moving these discoveries from the lab into the clinic. Sonoma Biotherapeutics, co-founded by immunologist Jeffrey Bluestone and now advised by Nobel laureate Fred Ramsdell, has been developing regulatory T cell therapies for autoimmune diseases like rheumatoid arthritis.
One promising approach takes regulatory T cells from a patient, copies them in large numbers in the lab, and puts them back into the body. Another method engineers these cells with a chimeric antigen receptor (CAR), creating what scientists call regulatory CAR T cells. CAR T cell therapy has already shown promise in cancer treatment, and researchers are now adapting it for autoimmune conditions and organ transplants.
Organ transplant rejection remains one of medicine’s biggest challenges. When a patient receives a donor organ, their immune system often attacks it as a foreign invader. Current anti-rejection drugs suppress the immune system broadly, leaving patients vulnerable to infections. Regulatory T cell therapies could train the immune system to accept the transplant without weakening its ability to fight real threats.
Research teams are also exploring gene therapy to correct Foxp3 mutations directly. For patients born with defective regulatory T cells, fixing the genetic root cause could mean a cure rather than a lifetime of symptom management.
A Win for Persistence and Curiosity
Perhaps one of the most inspiring parts of this story is how long it took. Sakaguchi spent years working on an idea most of his peers had abandoned. Brunkow and Ramsdell pursued a genetic mystery in a strain of mice that most researchers overlooked. None of them gave up.
When the Nobel Committee announced the award in October 2025, committee chair Olle Kämpe summed up the significance well: their discoveries have been decisive for our understanding of how the immune system functions and why we do not all develop serious autoimmune diseases.
For patients living with autoimmune conditions, that understanding is more than academic. It represents real hope for better treatments, fewer side effects, and possibly even cures. And for all of us, it serves as a powerful reminder that the human body still has secrets worth discovering.
My Personal RX on Supporting Your Immune System and Reducing Autoimmune Risk
As a doctor, I see autoimmune conditions more often than most people realize. Patients come to me with joint pain, chronic fatigue, skin rashes, and digestive problems that never seem to go away. Many of them feel frustrated because standard treatments only manage symptoms without getting to the root of the problem. What excites me about regulatory T cell research is that it points us toward smarter, more targeted solutions. But you do not have to wait for a clinical trial to start supporting your immune health. Simple daily habits can help keep your immune system balanced and reduce chronic inflammation. Here are my recommendations for protecting your body from immune system dysfunction.
- Move Your Body for at Least 30 Minutes Daily: Regular exercise reduces inflammatory markers in the blood and supports healthy immune function. Walking, swimming, yoga, or strength training all count.
- Get Quality Sleep Every Night: Poor sleep triggers inflammatory responses and weakens immune regulation. Sleep Max combines magnesium, GABA, 5-HTP, and taurine to calm your mind, balance neurotransmitters, and promote restorative REM sleep so your body can repair itself overnight.
- Manage Stress Before It Manages You: Chronic stress raises cortisol levels, which can throw your immune system off balance. Practice deep breathing, meditation, or journaling for at least 10 minutes a day.
- Know Which Supplements Your Body Needs: After age 40, nutrient gaps can affect energy, sleep, and immune function. Download my free guide, “7 Supplements You Can’t Live Without,” to learn which supplements matter most and how to spot quality products.
- Cut Back on Processed Foods and Refined Sugar: Both increase systemic inflammation and can disrupt the gut microbiome, making immune dysfunction more likely.
- Stay Hydrated Throughout the Day: Water supports every process in your body, including immune cell production and waste removal. Aim for at least eight glasses daily.
- Build Strong Social Connections: Loneliness and isolation increase inflammation and weaken immune response. Spend time with family and friends, join a community group, or volunteer.
- Talk to Your Doctor About Your Family History: If autoimmune conditions run in your family, schedule regular checkups and discuss screening options early. Prevention and early detection give you the best chance at staying healthy.
Sources:
Rocamora-Reverte, L., Melzer, F. L., Würzner, R., & Weinberger, B. (2021). The complex role of regulatory T cells in immunity and aging. Frontiers in Immunology, 11, 616949. https://doi.org/10.3389/fimmu.2020.616949
Raghavan, S., & Holmgren, J. (2004). CD4+CD25+suppressor T cells regulate pathogen induced inflammation and disease. FEMS Immunology & Medical Microbiology, 44(2), 121–127. https://doi.org/10.1016/j.femsim.2004.10.017









 Subscribe to Ask Dr. Nandi YouTube Channel
Subscribe to Ask Dr. Nandi YouTube Channel









