How many times does a patient need to say, “I know something is wrong,” before someone listens? Georgia O’Connor said it for 17 weeks.
She was a 25-year-old professional boxer—undefeated, fit, focused. She also lived with two chronic conditions that placed her at significantly higher risk for cancer. Yet despite repeated emergency visits, escalating pain, and specific warnings about her medical history, doctors told her it was “all in her head.” By the time she was finally diagnosed, her cancer had spread. She died less than four months later.
Georgia’s story is not an anomaly. Studies show that younger patients, particularly women, are disproportionately dismissed in clinical settings, often told they’re too young, too anxious, or simply “overreacting.” One major analysis found that even a four-week delay in cancer treatment can raise the risk of death by up to 8%. Georgia waited 17.
The Price of Being Ignored: Georgia O’Connor’s Final Months
Georgia O’Connor didn’t delay care. She didn’t ignore warning signs. In fact, she did everything a medically informed patient is supposed to do: she sought help early, voiced her concerns clearly, and identified herself as high risk. Still, for 17 weeks, she was dismissed by the very system meant to protect her.
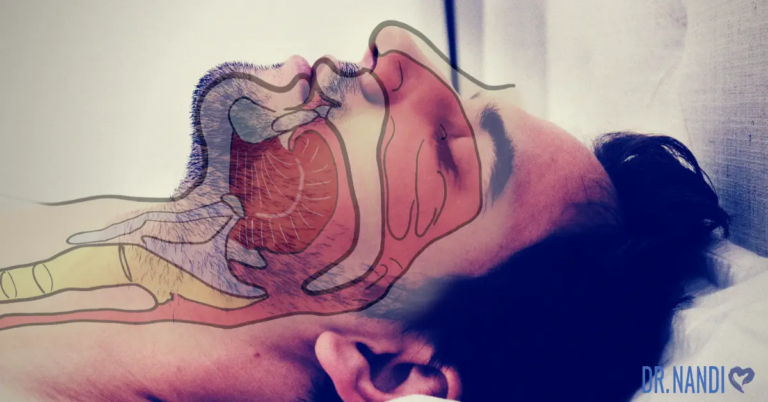
Beginning in October 2024, Georgia experienced persistent, severe pain. She visited emergency departments in Durham and Newcastle repeatedly, sometimes in such distress that she was “crying on the floor in agony,” as she later described. At every turn, she told healthcare professionals she suspected cancer. This wasn’t a vague concern—she had ulcerative colitis and primary sclerosing cholangitis (PSC), two well-established risk factors for gastrointestinal cancers. But she wasn’t believed. According to her, no imaging was ordered. No bloodwork was done. She was told it was “nothing.” One doctor even suggested it was “all in her head.”
When the diagnosis finally came in January 2025, it was exactly what she feared—and worse. The cancer had already metastasized. On top of that, scans revealed blood clots in her lungs, a life-threatening complication that, on its own, could have killed her. She announced the diagnosis on Instagram in a post that was raw, angry, and brutally honest. It was an indictment of a healthcare system that failed to take a young woman seriously, even as her condition deteriorated.

Georgia’s final months were a mixture of grit, heartbreak, and resilience. In March, she turned 25. In May, she married her partner Adriano, just 13 days before her death. Despite everything, she never stopped fighting. She vowed to pursue the best treatment possible and held on to hope, not just for herself, but for the possibility that her story might prevent this from happening to someone else.
The cost of being ignored wasn’t just a delay in diagnosis. It was the difference between a potentially treatable condition and a terminal one. It was the erosion of trust in a system. It was a preventable death in someone who was young, strong, and self-advocating, but not listened to.
Her Concerns Were Clinically Valid
Georgia O’Connor wasn’t guessing when she said, “I knew the risks.” She wasn’t catastrophizing. Her concerns were rooted in real, well-documented medical facts—facts any competent physician should recognize.
She lived with ulcerative colitis, a chronic inflammatory bowel disease. Over time, especially when extensive or poorly controlled, ulcerative colitis significantly increases the risk of developing colorectal cancer. According to long-standing clinical data, the longer someone has ulcerative colitis—especially when the entire colon is involved—the higher the likelihood of malignant transformation.
She also had primary sclerosing cholangitis (PSC), a rare liver disease that commonly coexists with ulcerative colitis. Importantly, PSC further multiplies the risk. Patients with both PSC and ulcerative colitis are not just at risk for colon cancer—they are also more prone to cholangiocarcinoma, a rare but aggressive cancer of the bile ducts. The combination of these two conditions is considered a high-risk profile in gastroenterology, and international guidelines recommend routine surveillance with imaging and lab work in these patients, even when they are asymptomatic.
Georgia wasn’t asymptomatic. She was in constant, worsening pain. She asked for scans. She asked for blood tests. She wasn’t just a young woman in discomfort—she was a young woman with two chronic, high-risk diseases presenting with new, severe symptoms. That should have immediately triggered diagnostic work-up, including imaging of the abdomen and pelvis, and possibly endoscopy or tumor marker testing.
Her medical risk wasn’t obscure. It was textbook. The British Society of Gastroenterology, the American Gastroenterological Association, and other major bodies all recognize this dual diagnosis as a red flag scenario. These patients don’t just deserve thorough evaluation—they require it. Failing to act isn’t just clinical negligence—it’s a disregard for established standard of care.
Georgia knew this. She said it out loud. She told her doctors that something serious was happening. What makes her story particularly painful is that her instincts were more medically sound than the judgment of those treating her.
The Deadly Cost of Diagnostic Delay in Young Adults
Georgia O’Connor’s story is tragic, but not rare. She was young, which should never be a reason to dismiss serious symptoms—but often is. In clinical settings, age can bias decision-making. Physicians may unconsciously assume that cancer is unlikely in a 20-something patient, especially one who appears otherwise healthy. This false sense of reassurance delays essential testing and can cost lives.
Multiple studies have highlighted this blind spot. Research published in Frontiers in Medicine found that younger adults are more likely to be misdiagnosed or have their symptoms minimized, especially when presenting with vague or non-specific signs like abdominal pain, fatigue, or bloating. For cancer specifically, early symptoms often overlap with benign conditions—especially in younger patients—making clinical intuition even more prone to error if objective testing isn’t done.
Delays in diagnosis don’t just affect peace of mind—they change outcomes. A major analysis in The BMJ showed that even a four-week delay in initiating cancer treatment increases mortality by 6% to 8%, depending on cancer type. Georgia waited 17 weeks before a proper workup was even started. That gap wasn’t just a delay in care—it likely meant the difference between a potentially curable condition and terminal disease.

It’s also important to recognize the added diagnostic burden placed on young women. Studies show that women, particularly those in their 20s and 30s, are more likely to be labeled as anxious, hormonal, or attention-seeking when they present with complex or persistent symptoms. The term “gaslighting” is often used to describe this experience—and Georgia used it herself. She said doctors made her feel like she was overreacting, that it was all psychological. By the time scans were finally performed, the cancer had spread and blood clots were present in her lungs.
When providers dismiss patients based on age or gender, they risk anchoring on the wrong diagnosis—or skipping the workup entirely. That’s not just poor medicine. In cases like Georgia’s, it’s deadly.
This isn’t just a call to improve bedside manner. It’s a demand for clinical vigilance. When a young patient says, “something isn’t right,” it’s not our job to reassure them with guesswork. It’s our job to prove they’re wrong—or act quickly if they’re not.
Honoring Georgia O’Connor Beyond the Headlines
Georgia O’Connor was more than a medical case and more than a headline. Before the illness, before the diagnosis, she was a rising star in British boxing—undefeated as a professional, decorated as an amateur, and known for her composure and discipline in the ring. But her strength extended far beyond sport.
She was also a musician, often sharing videos of herself playing guitar and singing. She was open about her struggles with chronic illness, mental health, and the emotional toll of high-level competition. And even as her cancer progressed, she didn’t retreat from public view. Instead, she posted with brutal honesty—about her pain, about being dismissed, about fighting to stay alive. Her voice was unfiltered and unflinching.
In her final months, she endured more than most people do in a lifetime: escalating symptoms, repeated medical rejection, a terminal diagnosis, and the loss of a pregnancy. Yet she still showed up—for herself, for her family, for those who followed her story. She turned 25. She got married. She smiled in hospital gowns. She made it clear that her story wasn’t just hers—it belonged to every young person who’s ever been told they were “too young” to be sick.
Georgia’s death has sparked an outpouring of grief and admiration from the boxing world and beyond. Friends, teammates, and champions like Ellie Scotney and Claressa Shields called her a light, a fighter, and a sister. But if we only remember her as the fighter who died young, we’ve missed the point.
She didn’t just want to be remembered—she wanted to be heard. Her legacy is a demand for better care, earlier action, and real accountability in how young people—especially women with chronic illnesses—are treated in the healthcare system. Honoring Georgia means listening to patients the first time. It means asking better questions. It means refusing to let preventable deaths be quietly folded into statistics.
Her story doesn’t end in the ring. It ends with a message loud enough that it still echoes: take people seriously when they say they’re in pain. She did. And she paid the highest price when no one else did.
My Personal RX on Tips for Recognizing Cancer Symptoms and Taking Action
As a physician, I often tell my patients that early detection is one of the most powerful tools we have in the fight against cancer. But the challenge is this: many early symptoms are subtle, easy to dismiss, or masked by everyday stress and fatigue. That’s why awareness—paired with proactive action—is key. Knowing what to look for and listening to your body can make all the difference. Just as important is creating an internal environment that’s less hospitable to disease through daily habits that support immune resilience, reduce inflammation, and nourish the body at every level. Prevention, early detection, and lifestyle support work best when they work together.
- Strengthen Immune Surveillance Through the Gut: A healthy gut supports immune detection of abnormal cells. MindBiotic delivers a powerful blend of probiotics, prebiotics, and Ashwagandha to help regulate immune activity, reduce inflammation, and keep your body alert to early changes.
- Eat with Prevention in Mind: The Mindful Meals cookbook includes 100+ anti-inflammatory, antioxidant-rich recipes using ingredients like turmeric, leafy greens, and cruciferous veggies—foods shown to help support cellular health and reduce cancer risk.
- Pay Attention to Unexplained Changes: Sudden weight loss, fatigue, persistent pain, or changes in skin, digestion, or appetite should never be ignored. These can be early signs of underlying disease.
- Know Your Family History—and Share It: Understanding your genetic risks can guide earlier or more frequent screenings. Always share your family’s cancer history with your healthcare provider.
- Don’t Ignore Digestive Symptoms: Bloating, blood in the stool, chronic constipation or diarrhea, or difficulty swallowing should always be evaluated—especially if symptoms persist.
- Track Menstrual and Hormonal Changes: Irregular periods, unusual bleeding, or breast changes should be discussed with your provider, as they could point to reproductive or hormonal cancers.
- Prioritize Regular Screenings: Mammograms, colonoscopies, Pap smears, skin checks, and blood tests save lives. Stay on schedule, even when you feel fine.
- Reduce Environmental Toxins Where Possible: Limit exposure to pesticides, plastics, synthetic fragrances, and processed foods. These compounds can contribute to DNA damage over time.
- Support Detox Pathways Naturally: Daily movement, deep sleep, hydration, and fiber-rich foods help your liver and lymphatic system clear out potential carcinogens efficiently.
- Trust Your Gut Instinct: If something feels “off” in your body, take it seriously. Early action—even just scheduling a checkup—can make a critical difference in outcomes.









 Subscribe to Ask Dr. Nandi YouTube Channel
Subscribe to Ask Dr. Nandi YouTube Channel









