Millions of people picked up vaping believing it was a safer alternative to smoking. Candy flavors, fruity scents, and sleek devices made the habit feel harmless, even trendy. But a growing body of evidence tells a very different story. What enters your lungs when you vape is not water vapor. It is a cocktail of chemicals, many of which scientists are only now beginning to understand. And some of the damage they cause cannot be undone. Flavored e-cigarettes, the most popular type among young users, are turning out to be far more dangerous than most people realize. What researchers are finding inside the lungs of vapers should make anyone holding a vape pen think twice before their next puff.
Vaping Is Not Just “Harmless Water Vapor”
A common myth about vaping is that you are inhaling nothing more than water and flavoring. In reality, every puff delivers a fine aerosol loaded with chemicals deep into your lung tissue.
E-cigarettes work by heating a liquid (called e-liquid or vape juice) until it becomes an aerosol you breathe in. Stephen Broderick, a lung cancer surgeon at Johns Hopkins, compares the delivery system to a medical nebulizer, a device that turns liquid medicine into a mist for patients with asthma or other lung conditions. A nebulizer is one of the most effective ways to deliver a substance directly into the lung tissue.
But instead of medicine, vaping delivers a mix of nicotine or THC, propylene glycol, vegetable glycerin, flavorings, and aromatic additives dissolved in an oily base. When heated, these ingredients produce additional byproducts that coat your lungs with every inhale.
A study from the University of North Carolina found that propylene glycol and vegetable glycerin, the two primary ingredients in most e-liquids, are toxic to cells. Even more concerning: the more ingredients an e-liquid contains, the greater the toxicity. Flavored varieties, which pack the most additives, cause the most cellular damage.
What Is Actually Inside Flavored Vape Juice
Flavored e-cigarettes owe their appeal to chemical additives that mimic the taste of fruits, candy, desserts, and menthol. But several of those chemicals are known to cause serious harm when inhaled.
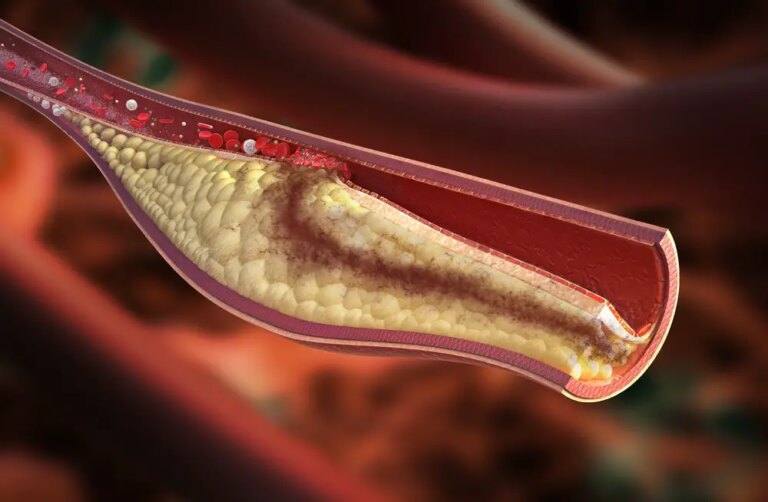
Diacetyl is one of the worst offenders. Food manufacturers use it to create a buttery flavor in products like microwave popcorn. When added to e-liquid, it deepens the taste profile. But when you inhale diacetyl, it causes inflammation in the smallest branches of your airways and can lead to permanent scarring. Your lungs were never designed to process food-grade chemicals through inhalation, and the results can be devastating.
Other dangerous chemicals found in e-cigarettes or produced when e-liquid is heated include formaldehyde, a toxic compound linked to lung and heart disease; acrolein, a chemical used as a weed killer that can cause acute lung injury and chronic obstructive pulmonary disease (COPD); benzene, a carcinogen found in car exhaust; and heavy metals like nickel, tin, and lead.
Vitamin E acetate deserves special mention. Used as a thickening agent in many e-liquids, it is safe to swallow as a supplement or apply to skin. But when vaporized and inhaled, it acts as an irritant deep inside the lung tissue. Investigators found vitamin E acetate in the lungs of patients hospitalized with severe vaping-related injuries.

Popcorn Lung: Permanent Damage from a Flavor Additive
One of the most alarming conditions linked to flavored vaping is bronchiolitis obliterans, better known as popcorn lung. Doctors first identified it when workers in popcorn factories started getting sick from inhaling diacetyl fumes. Now the same chemical sits inside millions of flavored vape cartridges.
Popcorn lung occurs when diacetyl damages the tiny airways in your lungs, causing inflammation and permanent scarring. Once that scarring sets in, breathing becomes difficult, and the damage cannot be reversed. No lasting treatment exists for bronchiolitis obliterans. Doctors can only manage symptoms like chronic coughing, wheezing, chest pain, and shortness of breath. A flavor additive designed to make your vape taste like mango or vanilla cream can cause irreversible scarring in your lungs.
Lipoid Pneumonia: When Oil Coats Your Lungs
Unlike traditional pneumonia caused by infection, lipoid pneumonia develops when fatty acids enter the lung tissue. Vaping-related lipoid pneumonia happens because e-liquid contains oily substances that, once inhaled, trigger an inflammatory response inside the lungs.
Symptoms include chronic cough, shortness of breath, and coughing up blood or blood-tinged mucus. And according to Broderick, there is no good treatment for lipoid pneumonia other than supportive care while the lungs attempt to heal on their own. Recovery depends entirely on one thing: identifying the cause and stopping it. For vapers, that means putting down the device. For many, the lung damage is already done by the time symptoms appear.
Collapsed Lungs in Young Vapers
Broderick reports seeing a surge of collapsed lungs (primary spontaneous pneumothorax) in younger patients at Johns Hopkins. A collapsed lung occurs when a hole forms in lung tissue and oxygen escapes into the body cavity.
Some people develop small air blisters at the top of their lungs, often during rapid growth in adolescence. On their own, these blisters rarely cause problems. But both smoking and vaping increase the risk of those blisters rupturing, causing lung collapse.
When Broderick asks these young patients about smoking, the answer is almost always the same: they do not smoke, but they do vape. His advice is clear: avoid both if you want to prevent a collapsed lung and the surgery that may follow.
Signs of a collapsed lung include sharp chest or shoulder pain, shortness of breath, and difficulty breathing. Mild cases may heal with oxygen treatment and rest, but severe cases require a chest tube or surgical repair.
Young Brains and Nicotine: A Dangerous Combination
Beyond lung damage, flavored e-cigarettes pose a serious threat to brain development in young users. Most e-liquids contain nicotine, one of the most addictive substances known.
Because the human brain does not finish developing until the mid-20s, teenagers and young adults face heightened risks from nicotine exposure. Nicotine rewires developing brains in ways that affect mood regulation, impulse control, attention, and learning. It also primes adolescent brains for addiction to other substances, including cocaine.
Flavored products make nicotine exposure worse because they attract younger users. Candy, fruit, and dessert flavors appeal directly to teens and tweens, turning what feels like a harmless treat into a fast track toward addiction. In 2019, 32% of Massachusetts high school students reported vaping in the past 30 days, and more than half had tried it at least once.
Some young people do not even realize they are addicted until they try to stop. Signs of nicotine dependence include strong cravings, anxiety when unable to vape, difficulty concentrating, irritability, and feeling like you need to vape just to feel normal.
Secondhand Vapor Is Not Safe Either
Many people assume that the cloud exhaled by a vaper is just harmless moisture. It is not. Secondhand e-cigarette emissions contain nicotine, ultrafine particles, diacetyl, benzene, volatile organic compounds, and heavy metals.
Both the U.S. Surgeon General and the National Academies of Science, Engineering, and Medicine have warned about the risks of breathing in secondhand vape aerosol. While the full health effects are still being studied, the known contents of that exhaled cloud are reason enough to avoid exposure, especially for children, pregnant women, and people with existing lung conditions.
Why Standard Treatment Has Not Changed in Decades
E-cigarettes have been sold in the United States for about a decade, and the FDA has not yet completed a systematic review of their effects on lung health. No e-cigarette has been approved by the FDA as a safe or effective tool for quitting smoking.
Meanwhile, the American Lung Association continues to raise alarms about the mounting evidence against e-cigarettes. A 2018 National Academies report reviewed over 800 studies and concluded that e-cigarettes both contain and emit several toxic substances. It also found moderate evidence that young e-cigarette users face increased risk of coughing, wheezing, and asthma flare-ups.
For anyone who took up vaping as a “healthier” alternative to cigarettes, the science paints a sobering picture. And for those who never smoked but started vaping for the flavors, the risks are real and growing.
What You Can Do Right Now
If you vape, the single most important step is to stop. Lung tissue can heal to some degree once the source of damage is removed, but certain conditions, like popcorn lung, cause permanent scarring that no treatment can reverse.
If you are a parent, talk to your children about vaping. Youth whose parents discuss the dangers of nicotine early and often are 50% less likely to use drugs, according to the National Council on Alcoholism and Drug Dependence. Learn what vaping devices look like, since many resemble USB drives, pens, or other everyday objects designed for discreet use.
If you experience chest pain, chronic cough, shortness of breath, or wheezing, see a doctor. Do not dismiss lung symptoms as normal, especially if you vape or have vaped in the past.
My Personal RX on Protecting Your Lung Health
Your lungs are under constant assault from environmental toxins, pollutants, and, for many people, the chemicals in e-cigarettes. Lung damage from vaping can be permanent, making prevention and early action essential. I always tell my patients that healthy lungs depend on what you breathe, what you eat, how you sleep, and how well your body manages inflammation. Even if you have never vaped, protecting your respiratory system should be a daily priority. Here is what I recommend:
- Quit Vaping and Smoking Immediately: No amount of flavored vapor is safe for your lungs. If you need help quitting, call 1-800-QUIT-NOW or text “Start My Quit” to 36072 for free, confidential coaching from trained specialists.
- Get Deep, Restorative Sleep Every Night: Your body repairs damaged tissue during deep sleep, including lung cells. Sleep Max combines magnesium, GABA, 5-HTP, and taurine to calm your mind and promote restorative REM sleep, giving your lungs the recovery window they need.
- Fill Your Nutrient Gaps: After 40, your body absorbs fewer key nutrients needed for immune function and tissue repair. Download my free guide, The 7 Supplements You Can’t Live Without, to learn which supplements matter most, which “healthy” foods may be misleading you, and how to spot quality products.
- Exercise to Strengthen Lung Capacity: Regular aerobic activity like walking, swimming, or cycling trains your lungs to work more efficiently and improves oxygen exchange. Aim for 30 minutes of moderate movement most days.
- Improve Indoor Air Quality: Open windows when possible, use air purifiers, and avoid burning candles or incense indoors. Clean air in your home gives your lungs a break from constant chemical exposure.
- Stay Hydrated: Water keeps the mucosal lining of your lungs thin, which helps them function better and clear out irritants. Aim for at least eight glasses per day.
- Talk to Your Kids About Vaping Early: Children as young as 11 are now exposed to e-cigarettes. Have honest, age-appropriate conversations about what vaping does to lungs and brains before peer pressure decides for them.
- See a Doctor If Symptoms Appear: Do not ignore chronic cough, chest tightness, wheezing, or shortness of breath. Early evaluation gives you the best chance at catching reversible damage before it becomes permanent.
Source:
Casey, A. M., Muise, E. D., & Alexander, L. E. C. (2020). Vaping and e-cigarette use. Mysterious lung manifestations and an epidemic. Current Opinion in Immunology, 66, 143–150. https://doi.org/10.1016/j.coi.2020.10.003
Amjad, M. A., Trujillo, D. O., Estrada-Y-Martin, R. M., & Cherian, S. V. (2025). E-Cigarette or vaping product Use-Associated Lung Injury: A Comprehensive review. International Journal of Environmental Research and Public Health, 22(5), 792. https://doi.org/10.3390/ijerph22050792










 Subscribe to Ask Dr. Nandi YouTube Channel
Subscribe to Ask Dr. Nandi YouTube Channel









