Imagine learning you have diabetes. Confusing enough. But then, you discover it’s not the type you thought. This was the reality for NSYNC’s Lance Bass, who initially received a diagnosis of type 2 diabetes, only to find out later that he actually has type 1.5 diabetes. Such misdiagnoses are surprisingly common, shedding light on a lesser-known form of the disease that blurs the lines between type 1 and type 2 diabetes.
It reveals itself stealthily, often masquerading as its more familiar counterparts and leading to treatment missteps. The nuances of this condition are not just a medical curiosity; they are a critical puzzle piece in understanding autoimmune diabetes in adults and refining approaches to diabetes care.
The Most Common Types of Diabetes We Know
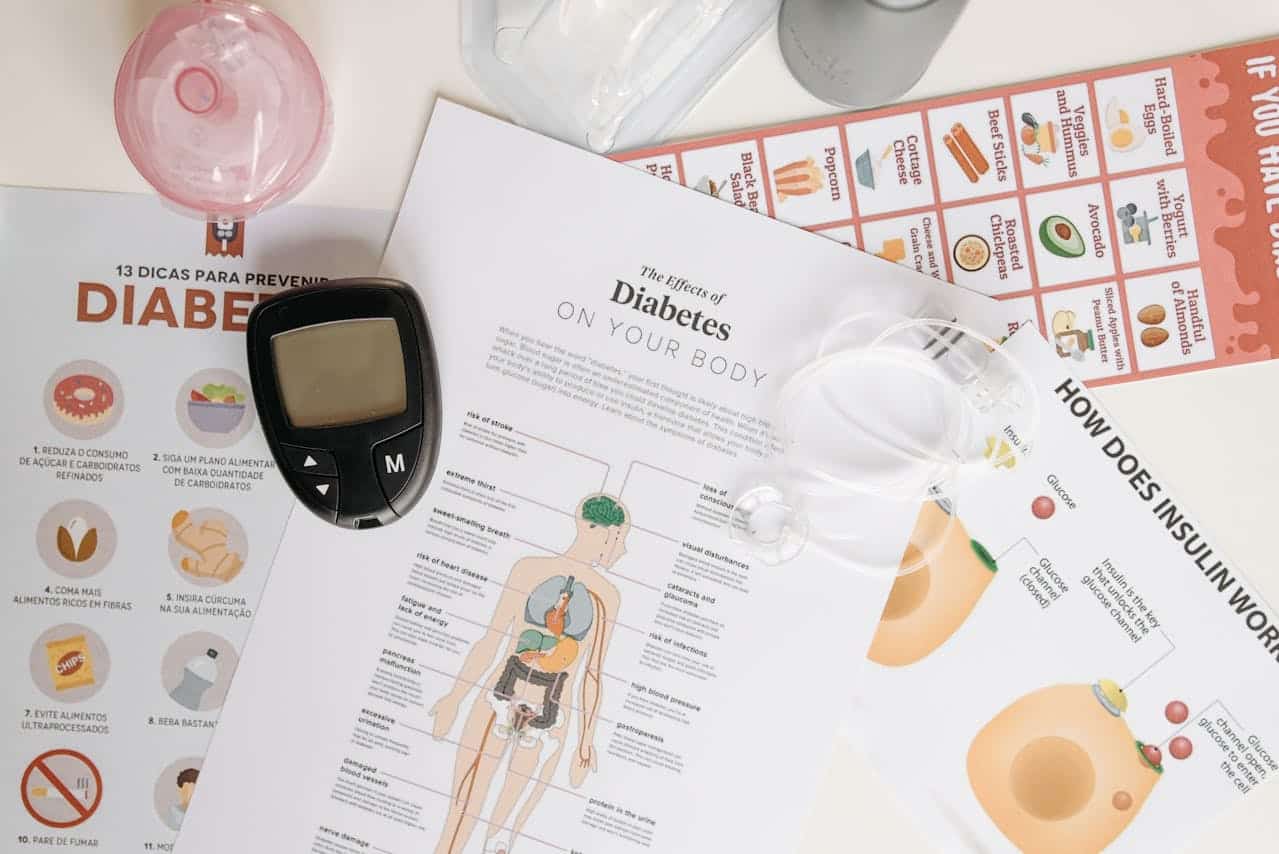
Diabetes mellitus, commonly referred to as diabetes, involves conditions that impact how your body converts food into energy. The name derives from Greek and Latin origins, with “diabetes” meaning to siphon or pass through and “mellitus” indicating sweetness, referring to the excess sugar found in the blood of those affected.
Globally, diabetes affects millions, with an estimated 529 million people worldwide and 38.4 million in the U.S. as of 2021. The condition centers on the metabolism of glucose, a type of sugar. When you consume carbohydrates, they are converted into glucose, which enters your bloodstream. In response, the pancreas releases insulin, a hormone that facilitates the transfer of glucose into cells, fueling them with energy.
There are several types of diabetes, but the most prevalent are type 1 and type 2. Type 1 diabetes is an autoimmune disorder where the immune system mistakenly attacks and destroys insulin-producing cells in the pancreas, resulting in little to no insulin production. It typically manifests in children or young adults, and managing it requires daily insulin administration.
Conversely, type 2 diabetes occurs as cells gradually become resistant to insulin. The pancreas struggles to produce sufficient insulin to counteract this resistance, which predominantly affects adults but is increasingly diagnosed in younger populations. Management strategies include dietary changes, increased physical activity, and potentially, medication and insulin therapy.

But What Is Type 1.5 Diabetes?
Type 1.5 diabetes, also known as Latent Autoimmune Diabetes in Adults (LADA), represents a form of diabetes that exhibits characteristics of both type 1 and type 2 diabetes.
This condition typically arises when the immune system mistakenly attacks pancreatic cells that produce insulin, similar to type 1 diabetes. However, unlike type 1, where insulin dependency is immediate, type 1.5 diabetes develops gradually, and individuals may not require insulin therapy right away. Most individuals diagnosed with type 1.5 diabetes will need insulin within five years of their diagnosis.
The onset of type 1.5 diabetes generally occurs in adults over the age of 30, which is later than the typical age for type 1 but younger than that most common for type 2 diabetes. This intermediate age of onset reflects its characteristics that bridge both types of diabetes.
Type 1.5 diabetes is associated with genetic and autoimmune risk factors similar to those seen in type 1 diabetes, including specific gene variants that predispose individuals to an autoimmune response against pancreatic cells. Additionally, lifestyle factors such as obesity and physical inactivity, typically linked with type 2 diabetes, also play a role in the development of type 1.5 diabetes. This dual influence makes it a unique and often misunderstood condition within the spectrum of diabetes.
Why Is Type 1.5 Diabetes Often Misdiagnosed?
Type 1.5 diabetes or LADA is commonly misdiagnosed, often as type 2 diabetes, affecting an estimated 4% to 12% of patients who are initially diagnosed with type 2.
The need for specific antibody tests to detect autoimmune markers is one primary challenge in diagnosing type 1.5 diabetes accurately. These tests, crucial for confirming the autoimmune aspect of diabetes, are not always conducted. Health professionals might not order these tests routinely due to cost constraints or a lack of awareness about their importance.
Moreover, type 1.5 diabetes primarily manifests in adults, which can lead to assumptions by medical professionals that any adult-onset diabetes is type 2, given its prevalence in this demographic. This can obscure the true nature of the condition, which, while similar to type 2 in its gradual progression, originates from an autoimmune response.
The case of NSYNC’s Lance Bass illustrates this diagnostic confusion. Initially diagnosed with type 2 diabetes, Bass was later correctly diagnosed with type 1.5 diabetes. His case highlights not only the commonality of such misdiagnoses but also the necessity of specialized testing.
Patients with type 1.5 diabetes can often manage their glucose levels initially without insulin, which can further complicate diagnosis. Their ability to produce enough insulin initially to manage blood glucose without medication can misleadingly present as type 2 diabetes, where insulin resistance rather than absence is often the issue.
The autoimmune destruction of pancreatic beta cells in type 1.5 diabetes is a slow process, leading to a gradual loss of insulin production and a corresponding increase in blood glucose levels. This slow progression means that patients can remain asymptomatic for years, delaying diagnosis until significant beta cell loss occurs.
How Is Type 1.5 Diabetes Diagnosed and Treated?
LADA can present variably in symptoms, ranging from increased thirst and frequent urination to fatigue, blurred vision, and unintentional weight loss. These symptoms might not initially raise alarms for type 1.5 diabetes, as they can be mild and are often similar to those of type 2 diabetes, leading to misdiagnoses.
Accurately diagnosing LADA involves a few critical steps. Initially, healthcare providers might suspect LADA in people who don’t have typical type 2 diabetes characteristics such as obesity or signs of insulin resistance, especially if they have another autoimmune condition or a family history of such conditions. Key diagnostic tests include:
- Autoantibody Tests: Checking for the presence of pancreatic autoantibodies is crucial as it indicates an autoimmune attack on insulin-producing cells.
- C-peptide Test: This test measures the level of C-peptide in the blood, which helps infer the body’s insulin production. Low C-peptide levels can suggest LADA as the body’s ability to produce insulin diminishes.
Treatment Approaches
Initially, type 1.5 diabetes might be managed with oral medications aimed at maintaining normal blood glucose levels. However, because these individuals eventually experience a decline in insulin production, transitioning to insulin therapy becomes necessary.
It’s important to start insulin treatment early to manage glucose levels effectively and prevent diabetes-related complications such as kidney disease, cardiovascular issues, nerve damage, and eye disease.
Lifestyle Modifications
In addition to medical treatment, lifestyle changes are recommended, similar to those for managing type 2 diabetes. These include maintaining a healthy weight, staying active, following a balanced diet, and quitting smoking. These measures can help manage the condition initially but are usually insufficient alone as the disease progresses.
Early Intervention and Management
Regular monitoring of blood glucose levels is essential for people with LADA, especially as the disease progresses. Patients may need to adjust their insulin dosage based on frequent blood sugar testing results.
Early and accurate diagnosis followed by prompt insulin therapy can significantly improve management outcomes for people with LADA. Early initiation of insulin can help preserve beta-cell function and potentially slow the progression of the disease, reducing the risk of severe hypoglycemia and stabilizing the patient’s metabolic state. Patients often report an improvement in energy, strength, and overall well-being once insulin treatment begins.
My Personal RX on Diabetes Prevention and Management
Diabetes is a significant health concern that affects millions globally, but the good news is that with the right lifestyle and dietary choices, it can often be prevented. Even after a diagnosis, by adopting certain practices, individuals can manage their condition effectively and continue to lead a joyful and fulfilling life. As a doctor, I can’t stress enough the power of prevention through lifestyle adjustments and also the importance of proper management after a diagnosis.
- Prioritize Regular Physical Activity: Exercise plays a crucial role in maintaining healthy blood sugar levels. It helps increase insulin sensitivity, which means your cells are better able to use the available sugar in your bloodstream. Aim for at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous activity each week.
- Adopt a Low-Glycemic Diet: Focus on foods that have a low glycemic index, which have a slower impact on your blood glucose levels. Foods rich in fiber such as whole grains, legumes, nuts, seeds, fruits, and vegetables are excellent choices.
- Stay Hydrated: Drinking enough water is important for everyone, but it’s especially crucial for individuals managing diabetes. Proper hydration helps regulate blood sugar levels and aids in kidney function, helping to flush out excess glucose through urine. Aim for clear or pale-yellow urine as a sign of good hydration.
- Incorporate MetaBurn for Weight Management: If you’re at risk of developing diabetes or managing your weight after a diagnosis, MetaBurn can assist in enhancing your metabolism and supporting healthy weight loss. A healthy weight can significantly improve blood sugar management and reduce the risk of complications.
- Monitor Your Health Regularly: Regular check-ups with your healthcare provider are essential for monitoring your blood sugar levels and managing your diabetes effectively. Early detection of potential complications can greatly improve the outcomes.
- Manage Stress Effectively: Stress can affect blood sugar levels. Techniques like meditation, yoga, and deep breathing can help manage stress and have a positive impact on your overall health.
- Stay Educated with Resources Like the Diabetic Desserts Cookbook: Managing diabetes doesn’t mean you have to give up enjoying food. My free Diabetic Desserts Cookbook provides recipes that are tailored to be lower in sugar and carbs, allowing you to enjoy sweets without significantly impacting your blood sugar levels. This can be a great way to maintain a sense of normalcy and satisfaction in your diet.
- Sleep Well: Adequate sleep is crucial for blood sugar control and overall health. Lack of sleep can disrupt important metabolic hormones.
- Quit Smoking and Limit Alcohol: Smoking and excessive alcohol consumption can worsen the complications of diabetes. Quitting smoking and limiting alcohol intake are important steps in managing your condition.
- Stay Connected: Joining a support group or community for people with diabetes can provide emotional support and practical tips for managing your condition. Knowing you are not alone can be very empowering.
Sources:
- Ong, K. L., Stafford, L. K., McLaughlin, S. A., Boyko, E. J., Vollset, S. E., Smith, A. E., Dalton, B. E., Duprey, J., Cruz, J. A., Hagins, H., Lindstedt, P. A., Aali, A., Abate, Y. H., Abate, M. D., Abbasian, M., Abbasi-Kangevari, Z., Abbasi-Kangevari, M., ElHafeez, S. A., Abd-Rabu, R., . . . Vos, T. (2023). Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the Global Burden of Disease Study 2021. The Lancet, 402(10397), 203–234. https://doi.org/10.1016/s0140-6736(23)01301-6
- Diabetes Basics. (2024, May 15). Diabetes. U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/about/index.html
- Rajkumar, V., & Levine, S. N. (2024, March 1). Latent autoimmune diabetes. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK557897/
- Sobhan, A. (2024, August 1). Lance Bass Reveals He Has Type 1.5 Diabetes: Here’s What That Means. People.com. https://people.com/lance-bass-reveals-he-has-type-1-5-diabetes-8687391









 Subscribe to Ask Dr. Nandi YouTube Channel
Subscribe to Ask Dr. Nandi YouTube Channel









