Nighttime light flooding American communities may increase Alzheimer’s disease risk, particularly for people under 65, according to research analyzing Medicare data and NASA satellite measurements. Scientists at Rush University Medical Center tracked Alzheimer’s prevalence across US states and counties from 2012 to 2018, comparing disease rates with outdoor light intensity captured by satellites. States with the brightest nighttime skies showed higher Alzheimer’s rates than the darkest states. Most striking results appeared in people under 65, where light pollution correlated more strongly with Alzheimer’s than any other risk factor studied, including diabetes, high blood pressure, obesity, depression, or alcohol abuse. For older adults, nighttime light is linked to Alzheimer’s more closely than alcohol abuse, chronic kidney disease, heart failure, and several other known risks, though cardiovascular factors like stroke showed stronger associations. Dr. Robin Voigt from Rush University Medical Center has spent over a decade studying how circadian rhythm disruption harms health, making her pleased but unsurprised by findings connecting outdoor lighting to brain disease.
How Light Pollution Scrambles Your Internal Clock
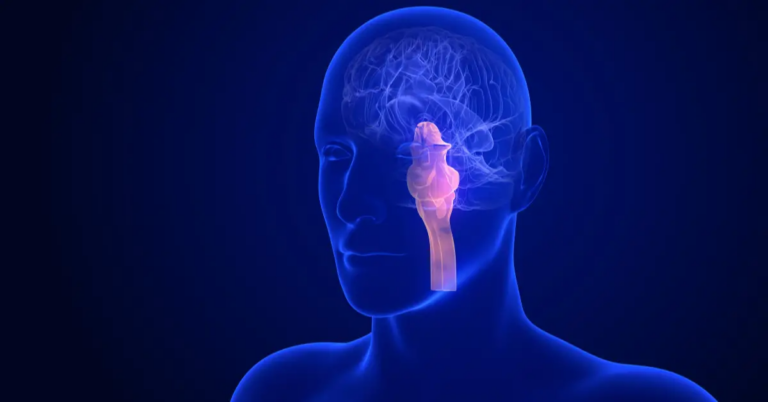
Light serves as the strongest factor influencing circadian rhythms, the 24-hour biological cycles controlling sleep, hormone production, metabolism, and countless other processes. Exposure to bright light at night confuses internal clocks evolved to sync with natural sunrise and sunset patterns. Artificial lighting tells the brain it’s still daytime when darkness should signal rest and cellular repair.
Circadian rhythms regulate much of biology and behavior throughout the body. When disrupted, consequences cascade through multiple systems. Sleep quality deteriorates first, but metabolic dysfunction, immune suppression, mood disorders, and now apparently neurodegeneration follow. Previous research linked light pollution to obesity, cancer risk, and metabolic problems. This study represents the first to connect outdoor nighttime light specifically to Alzheimer’s disease prevalence.
Dr. Voigt hypothesized that circadian disruption drives the Alzheimer’s connection. Bodies expect darkness during night hours to trigger melatonin production, lower body temperature, and activate repair mechanisms. Constant light exposure short-circuits these processes. Brain cells accumulate damage without adequate nighttime recovery periods. Toxic proteins that normally get cleared during sleep build up instead, potentially contributing to Alzheimer’s pathology.

What Researchers Found in 48 States
Scientists collected Medicare health insurance data tracking Alzheimer’s disease prevalence from 2012 through 2018. They cross-referenced medical records with NASA satellite measurements of outdoor nighttime light intensity across all US states except Alaska and Hawaii. County-level analyses provided a more detailed picture than state averages alone.
The states were divided into five groups from darkest to brightest based on average nighttime light exposure. Analysis revealed statistically significant differences in Alzheimer’s prevalence between groups. Darkest states showed lower disease rates than brightest states. Pearson correlation analysis confirmed positive relationships between light intensity and Alzheimer’s prevalence across all years examined.
County data told similar stories with even greater precision. Within individual states, counties with higher light pollution showed elevated Alzheimer’s rates compared to darker counties in the same state. Using counties containing each state’s largest city, researchers analyzed 45 counties plus Washington, DC, dividing them into four groups from darkest to brightest. Results replicated state-level findings, lending confidence to conclusions.
Linear mixed models accounting for repeated measurements over years confirmed associations held across demographics. Effects appeared in both sexes, all age groups, and every racial/ethnic category except Asian Pacific Islanders, where the sample size may have limited statistical power. Stronger regression coefficients appeared in certain ethnic groups, particularly Native Americans, though reasons remain unclear and deserve further investigation.
Why Young People Face Greatest Risk
Results for people under 65 proved particularly striking. Among this younger population, nighttime light intensity was associated with Alzheimer’s prevalence more strongly than all other disease risk factors examined. Diabetes, hypertension, obesity, depression, chronic kidney disease, heart failure, stroke, atrial fibrillation, hyperlipidemia, and alcohol abuse all showed weaker correlations with young-onset Alzheimer’s than outdoor light exposure.
Young-onset dementia remains relatively rare compared to late-life disease but devastates families when diagnosis strikes people during prime working and parenting years. Understanding risk factors for early Alzheimer’s matters because interventions targeting younger populations could prevent decades of disease burden.
Researchers struggle to explain why under-65 populations appear more vulnerable to nighttime light effects. Literature shows that individual differences in light sensitivity exist. APOE genotype, a factor influencing early-onset Alzheimer’s risk, affects how bodies respond to biological stressors, including oxidative stress. Perhaps genetic variations make some younger people particularly susceptible to circadian disruption from artificial light.
Modern lifestyles expose younger generations to more intense indoor and outdoor light than previous generations experienced. Smartphones, tablets, computers, and televisions add to outdoor light pollution in creating near-constant light exposure. Cumulative effects over decades might manifest as earlier disease onset in susceptible individuals.
Light Pollution’s Growing Footprint
Most people living in urban and suburban areas cannot see natural celestial light anymore. Light pollution affects as much as 80 percent of the global population. Artificial outdoor lights provide safety, convenience, and aesthetics by deterring crime, illuminating roadways, and highlighting landscaping. However, excessive artificial light at night from poorly shielded or overly bright fixtures creates pollution with ecological, behavioral, biological, and health consequences.
The study data spanned 2012 through 2018. During this period, states showed trends toward decreased nighttime light, dropping from a baseline of 100,000 units in 2012 to 96,890 units in 2018. The pandemic further reduced nighttime light exposure, reaching the lowest levels in 2020. Despite 17 states passing legislation designed to reduce light pollution, nighttime light hit its highest recorded levels in 2022 at 103,500 units.
Increased nighttime light could potentially impact Alzheimer’s incidence and prevalence going forward if associations prove causal. Rising light pollution runs counter to public health interests when research suggests environmental lighting influences neurodegenerative disease risk.
Mechanisms Linking Light to Brain Damage
Multiple pathways could explain how nighttime light exposure promotes Alzheimer’s development or progression. Sleep disruption represents the most obvious mechanism. Extensive literature documents that light exposure at night interferes with sleep quality and duration. Sleep disruption activates microglia and astrocytes, promotes inflammation, impairs clearance of amyloid beta proteins through the glymphatic system, causes neuron loss in the cortex and hippocampus, and leads to hippocampal atrophy.
Meta-analysis of 27 observational studies found that people with sleep problems face a higher risk of cognitive impairment and Alzheimer’s compared to those who sleep well. Sleep provides crucial time for brain cleaning processes that remove toxic protein buildup characteristic of Alzheimer’s pathology.
Circadian rhythm disruption may operate upstream of sleep problems. Light at night directly disrupts circadian rhythms, and sleep quality reflects one output of healthy circadian function. Changes in circadian rhythms often precede Alzheimer’s symptoms in humans, suggesting that environmental factors disrupting body clocks might contribute to disease development years before diagnosis.
Circadian disruption increases risk for diseases that themselves raise Alzheimer’s risk, including obesity, diabetes, and depression. Light exposure at night could promote Alzheimer’s indirectly by causing metabolic and mood disorders that damage brain health.
Biochemical changes provide another mechanism. Mouse studies show dim light during dark periods increases production of interleukin-1β, a pro-inflammatory cytokine associated with Alzheimer’s. Light exposure also decreases brain-derived neurotrophic factor in the hippocampus, a brain region critical for memory. Low BDNF levels precede cognitive impairment in humans, making this finding particularly relevant.
What Study Limitations Mean
Several important limitations deserve mention. Medicare data include only people enrolled in Medicare Part A and Part B, excluding those with Medicare Advantage or partial coverage. About 45 percent of Medicare beneficiaries were excluded, meaning the data don’t represent comprehensive population coverage.
Medicare records show current residences, which may not reflect lifelong exposure patterns. Causality requires understanding where people lived throughout their lives, not just where they reside when diagnosed. The study examined prevalence rather than incidence, making temporal relationships harder to establish.
Satellite measurements captured outdoor light only. Indoor light exposure from televisions, computers, and phones matters critically but wasn’t included. However, living in areas with intense outdoor nighttime light correlates with shorter sleep duration, increased daytime sleepiness, and dissatisfaction with sleep quality, suggesting outdoor light meaningfully impacts biology even when indoor exposure isn’t measured.
County and state averages mask individual variation in actual light exposure. Some people living in bright areas use blackout curtains and minimize light effectively. Others in darker areas may still experience high indoor light exposure. Individual-level data collection would provide a more precise understanding of dose-response relationships.

5 Simple Steps to Reduce Nighttime Light Exposure
You have more control over your light environment than you might think, and the most effective strategies are often the simplest ones.
• Remove Outdoor Light Sources: Dr. Voigt recommends practical interventions to minimize outdoor light entering homes. Remove unnecessary outdoor lights or swap standard bulbs for warmer color temperatures that emit less blue light. Blue wavelengths most strongly suppress melatonin and disrupt circadian rhythms.
• Install Blackout Solutions: Install blackout curtains in bedrooms to block external light sources. Complete darkness during sleep hours allows maximal melatonin production and circadian rhythm alignment. Eye shades provide portable blackout options, especially helpful when sharing beds with partners who watch television or use light-emitting devices.
• Manage Indoor Evening Light: Indoor light management matters equally. Dim lights during evening hours. Use amber or red bulbs in bedroom lamps. Activate blue light filters on phones, tablets, and computers. Stop screen time at least one hour before bed. Create consistent sleep schedules with regular bedtimes and wake times that reinforce natural circadian patterns.
• Advocate for Community Action: Community-level interventions could reduce light pollution, benefiting entire neighborhoods. Shield outdoor fixtures to direct light downward rather than upward into the sky and sideways into homes. Use motion sensors so lights activate only when needed rather than blazing constantly. Advocate for local ordinances limiting outdoor lighting intensity and requiring shielding on commercial fixtures.
• Prioritize Circadian Health: Protecting your circadian rhythms takes time and consistent practice because you’re rewiring biological responses that evolved over millennia. Be patient with yourself as you build these new light hygiene patterns.
My Personal RX on Protecting Your Brain From Light Pollution
Modern life bathes us in constant artificial light that evolution never prepared our bodies to handle. Brains expect darkness during nighttime hours to trigger repair mechanisms and clear toxic proteins. Circadian rhythm disruption from excessive light creates cascading problems throughout your body and brain. While research linking outdoor light pollution to Alzheimer’s remains preliminary and needs confirmation through additional studies, protecting your circadian rhythms offers proven benefits for sleep, metabolism, mood, and overall health regardless of dementia risk. You cannot control streetlights or neighbors’ security floods, but you can control light entering your home and personal light exposure patterns. Small changes compound over decades into meaningful protection for brain health. Sleep quality alone justifies reducing nighttime light exposure since poor sleep accelerates cognitive decline through multiple pathways. Your brain performs essential maintenance during sleep that cannot happen elsewhere. Giving your brain proper darkness to work in represents basic preventive care that costs nothing.
- Support Circadian Health Through Gut Balance: Gut microbiome influences circadian rhythms through metabolite production and immune signaling. MindBiotic provides probiotics, prebiotics, and Ashwagandha KSM 66 that support healthy circadian function, reduce inflammation, and improve stress resilience that protects brain health.
- Eat to Support Brain Repair Processes: Nutrient-dense foods provide building blocks for nighttime cellular repair. Mindful Meals cookbook offers 100+ doctor-approved recipes rich in antioxidants, omega-3 fatty acids, and brain-protective compounds that support cognitive health and reduce neuroinflammation.
- Install Complete Bedroom Darkness: Invest in blackout curtains or shades that block all external light. Even small amounts of light during sleep suppress melatonin production and disrupt circadian rhythms that regulate brain cleaning processes.
- Use Warm-Colored Evening Lighting: Replace bright white bulbs with warm amber or red bulbs in evening spaces. Blue wavelengths most strongly disrupt melatonin production, while warmer colors allow circadian rhythms to prepare for sleep.
- Eliminate Bedroom Electronics: Remove televisions, computers, and phones from bedrooms or keep them in drawers. Glowing displays and notification lights create light exposure throughout the night that fragments sleep and prevents deep restorative stages.
- Wear Blue Light Blocking Glasses: Don amber-tinted glasses two to three hours before bedtime when using screens or under bright lights. Blue light blocking lenses filter wavelengths that most strongly suppress melatonin and delay sleep onset.
- Get Bright Morning Light Exposure: Step outside within 30 minutes of waking for at least 10 minutes. Morning light exposure strengthens circadian rhythms and improves nighttime melatonin production, creating healthier sleep-wake cycles.
Source:
Voigt, R. M., Ouyang, B., & Keshavarzian, A. (2024). Outdoor nighttime light exposure (light pollution) is associated with Alzheimer’s disease. Frontiers in Neuroscience, 18, 1378498. https://doi.org/10.3389/fnins.2024.1378498








 Subscribe to Ask Dr. Nandi YouTube Channel
Subscribe to Ask Dr. Nandi YouTube Channel









