Diabetes isn’t a one-size-fits-all condition. While many are familiar with Type 1 and Type 2, even Type 1.5, researchers have long known that the disease presents in more than a dozen distinct ways. Now, the International Diabetes Federation has officially recognized a new subtype: Type 5 diabetes, also known as malnutrition-related diabetes mellitus (MRDM). This classification sheds light on a health crisis that has remained largely invisible in global discourse—and it demands a treatment strategy distinct from other forms of diabetes.
The Basics: How Type 5 Diabetes Is Different
Unlike Type 1, which stems from autoimmune destruction of insulin-producing cells, or Type 2, which is often tied to insulin resistance and metabolic factors, Type 5 diabetes arises from chronic undernutrition during early life. Specifically, a long-term lack of nutrients—either in utero or during early childhood—impairs the development of the pancreas. The result? A smaller or dysfunctional pancreas that simply can’t produce enough insulin.
This form of diabetes typically develops before age 30 and has now been confirmed to affect 20 to 25 million people worldwide, particularly in low-income regions of Asia and Africa, where food insecurity and childhood malnutrition are more prevalent.
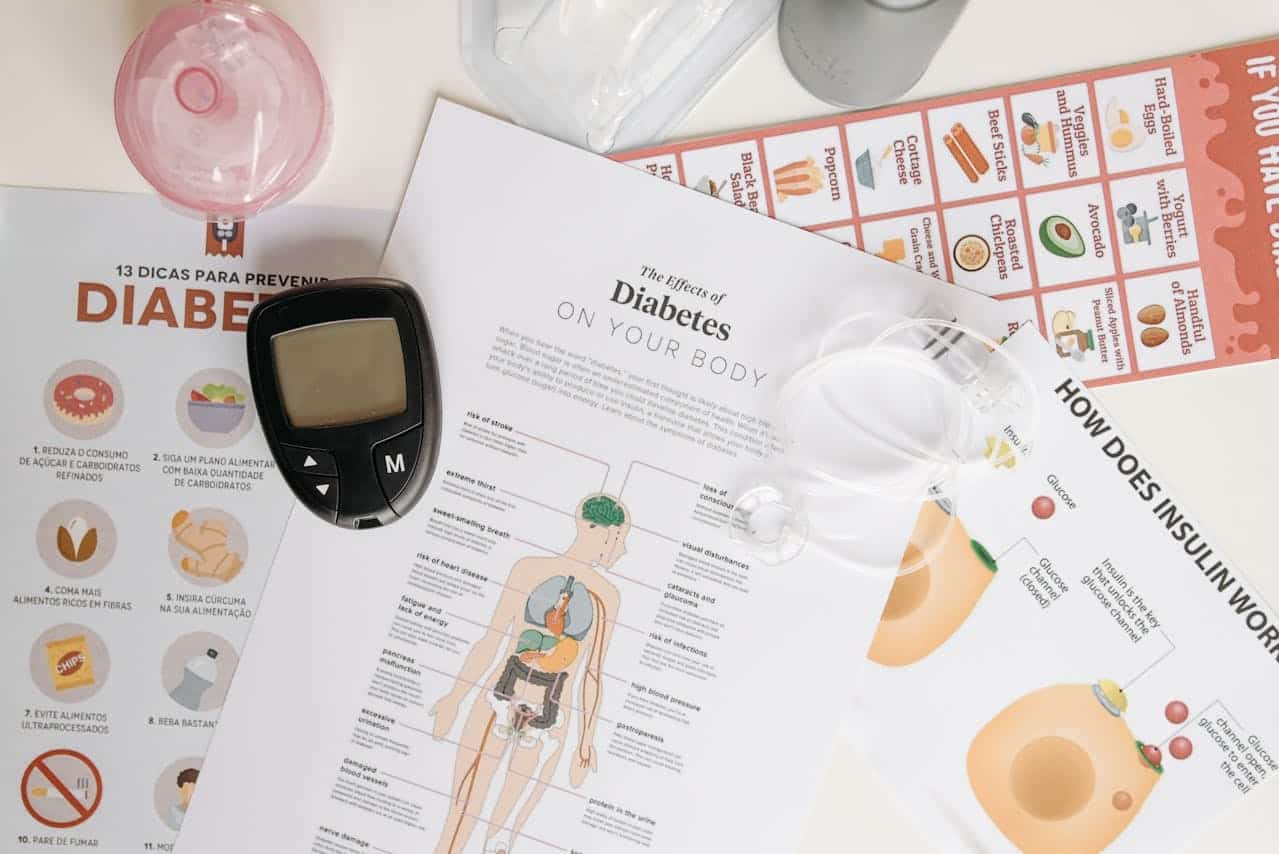
Early Warning Signs You Shouldn’t Ignore
Recognizing Type 5 diabetes can be tricky, especially since its symptoms often overlap with signs of long-term nutritional deficiencies. Rather than presenting in an obvious or acute way, the condition can slowly develop and mimic other forms of diabetes.
Here are some signs to be aware of:
- Constant thirst or dry mouth
- Needing to urinate more often than usual
- Tiredness that doesn’t improve with rest
- Vision that becomes blurry or hazy
- Cuts and scrapes that take a long time to heal

In addition to these classic diabetes symptoms, people with Type 5 often show physical evidence of early-life undernourishment, such as:
- Noticeably low weight for their age or height (BMI under 18.5)
- Stunted growth or delayed development
- Thinning hair or skin changes
- Swollen or enlarged salivary glands
This overlap in symptoms can make it easy to mistake Type 5 for Type 1 diabetes. But understanding these nuanced differences is key to getting the right diagnosis and treatment.
Diagnosing a Silent Crisis
In resource-limited settings, diagnostic tools are often unavailable, which complicates proper identification. Blood glucose tests and A1C tests can confirm elevated blood sugar levels, but without more specific testing (such as antibody screens or C-peptide levels), distinguishing Type 5 from Type 1 can be challenging.
However, there are some clues. Patients with Type 5 diabetes often lack ketones in their urine at diagnosis (a hallmark of Type 1 diabetes) and show signs of early-life malnutrition. A low BMI and diagnosis before the age of 30 are also strong indicators.
Causes: The Role of Early Nutrition
Studies have shown that a low-protein diet during pregnancy and adolescence in animal models results in poorly developed pancreases. In humans, early-life nutritional deficits impair the body’s ability to develop adequate insulin-producing beta cells.
This form of diabetes isn’t caused by autoimmunity or insulin resistance. Instead, it represents a functional insulin deficiency due to insufficient pancreas development. As a result, insulin must often be administered to prevent complications, despite the absence of autoimmune factors.
Complications: Similar to Other Forms, but with Added Burden
Like other types of diabetes, Type 5 can lead to serious complications if left untreated:
- Heart disease
- Kidney failure
- Nerve damage
- Vision loss
But because this type affects underserved populations with limited healthcare access, the complications can be more severe and harder to manage.

Treatment: A Different Strategy Required
While insulin therapy remains the primary treatment for managing blood sugar, researchers are actively exploring alternative oral medications that might better suit patients with Type 5 diabetes.
What makes this form particularly challenging is the coexistence of malnutrition. A patient managing Type 5 diabetes is not just balancing insulin levels but also addressing ongoing nutrient deficiencies, low muscle mass, and compromised immunity.
Effective management must therefore include:
- Nutritional support
- Blood sugar monitoring
- Safe insulin access
- Regular follow-up care
Rethinking Diabetes on a Global Scale
The recognition of Type 5 diabetes marks a major step forward in understanding diabetes as a diverse group of diseases, not a singular condition. This reclassification not only improves diagnosis but also shifts the focus toward better treatment options and health equity, especially in low- and middle-income nations.
As medical science evolves, this new understanding encourages policymakers, healthcare providers, and researchers to pay attention to the social determinants of health—and address malnutrition as a critical factor in chronic disease prevention.
My Personal RX: Recognizing and Managing Type 5 Diabetes
Seeing the emergence of Type 5 diabetes reminds us that global health is deeply tied to nutrition, access, and education. To help those living with or at risk of this condition, we must adopt a holistic approach that addresses not just the blood sugar imbalance but the roots of the issue: early-life undernutrition.
Here are my personal recommendations to support healthy blood sugar and improve nutrition, especially in underserved populations:
- Prioritize Balanced Nutrition Early: If you’re expecting or caring for a child, ensure their diet includes high-quality protein, healthy fats, and essential micronutrients. This supports pancreatic development and long-term metabolic health.
- Stay Informed on Diabetes Variants: Not all diabetes is the same. Understanding the differences can help you or your loved ones seek the right care. Knowledge is power.
- Use MindBiotic to Support Gut-Immune Health: Chronic malnutrition weakens the gut lining and immune system. MindBiotic is a unique blend of probiotics, prebiotics, and adaptogens that promotes better digestion, nutrient absorption, and mental clarity.
- Strengthen Daily Meals with Mindful Meals: For those recovering from undernutrition or managing diabetes, nutrient-dense, balanced meals are essential. Mindful Meals offers clean, whole food-based options that support blood sugar regulation and satiety.
- Advocate for Nutrition Programs in Your Community: Whether through schools, local clinics, or food banks, community-led nutrition efforts can make a real difference in preventing chronic diseases linked to malnutrition.
- Watch for Symptoms Beyond Weight: Low body weight alone isn’t always healthy. Look for fatigue, slow healing, and glucose issues that may indicate deeper health concerns.
- Talk to Your Doctor About Testing: If you or someone you know has diabetes and a history of malnutrition, ask about tests that can differentiate Type 5 from Type 1 or 2. This ensures the most effective treatment.
- Ensure Reliable Insulin Access: Advocacy efforts to improve global access to insulin can save lives. Support organizations that deliver essential diabetes care to underserved regions.
- Avoid Over-Supplementing Without Guidance: Nutritional supplements can help, but overuse or incorrect use can cause harm. Always consult a provider.
- Read to Empower Yourself: My book, Heal Your Gut, Save Your Brain, explores how nutrition and gut health influence everything from metabolism to mental wellness. A must-read for those managing or preventing chronic conditions.








 Subscribe to Ask Dr. Nandi YouTube Channel
Subscribe to Ask Dr. Nandi YouTube Channel









